- Amendment / Review History
- Strategic Statement
- Risk Assessment
- Education and Training
- Individual Accountability and Responsibility
- Standard Infection Control Precautions
- List of Potentially Infected Substances
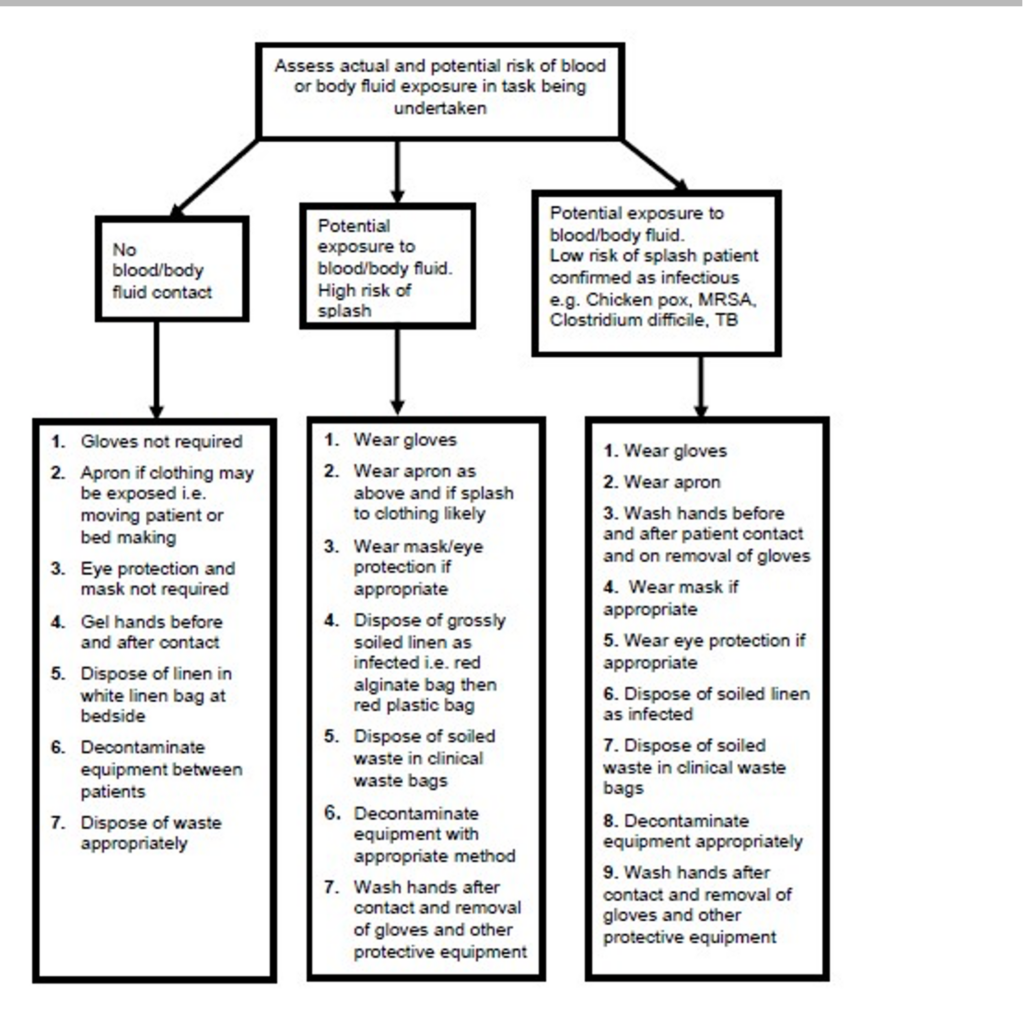
- Risk Assessment Guide for Selection of Protective Equipment Based on Risk of Exposure to Blood / Body Fluid
- Personal Protective Equipment (PPE)
- What to Wear and When
- Types of PPE
- Procedure for Patient Transport Services
- Vehicle Cleaning
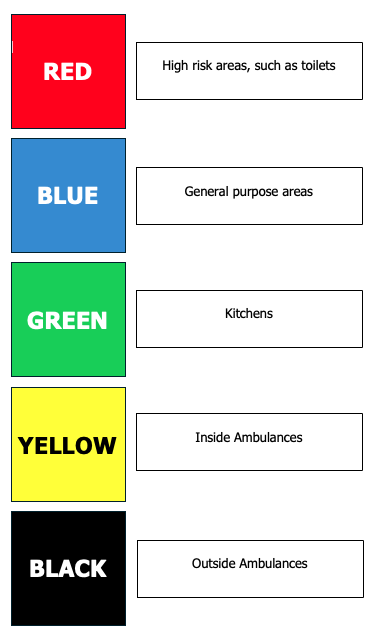
- Cleaning Materials and Equipment Colour Coding
| Author: | Jono Erodotou |
| Responsibility: | All Staff |
| Effective Date: | 01 June 2024 |
| Review Date: | 30th May 2025 |
| Approved By: | |
| Version Number: | 01 |
Amendment / Review History #
| Date | Author | Comments |
|---|---|---|
Strategic Statement #
The risk of transmitting healthcare associated infections (HCAIs) and other contagious pathogens to our patients, our colleagues, our families and ourselves is a controllable risk, and a risk that can be substantially and effectively reduced through the application of basic infection prevention and control procedures. The K4 Medical Services Cleanliness and Infection Control policy is intended to provide assurance that the standards of infection prevention and control are met, by respecting the patient’s right to a clean, modern environment and by our staff’s right to safe working conditions, by following best and evidence based practice This policy is intended to set out K4 Medical Service’s commitment to, and provisions for, reducing the incidence of HCAIs, and reducing the opportunities that the organisms responsible have to cause infections. This policy is designed to provide overarching assurances that the care we undertake as a private health care provider is delivered as safely as possible, ensuring that all reasonable steps are taken to minimise the risk of cross infection.
Risk Assessment #
In accordance with health and safety requirements, where suitable and sufficient assessment of risks requires appropriate action to be taken, evidence must be available on compliance with the Health and Social Care Act 2008 or where appropriate, justification of a suitable better alternative Infection prevention and control risks to staff patients and the public must be identified in all aspects of the responsibility of K4 Medical Services activity. K4 Medical Services has a responsibility to protect staff patients and the public as far as ‘reasonably practicable’. Actions must be taken to identify and avoid risks with the potential to cause harm.
Education and Training #
All new employees have infection control training including hand hygiene during the induction programme. All staff are required to complete a mandatory annual infection control update, this must include annual hand hygiene refresher for ambulance staff. Training will be provided by K4 Medical Services in the event of new skill requirements such as the introduction of new products or new evidence-based guidance on clinical practice. Staff will receive training when specific issues arise as part of an action plan or risk assessment e.g. following an infection control incident or as a result of poor compliance. The Training Manager is responsible for developing and updating K4 Medical Service’s training needs analysis to ensure it reflects the requirements of the Health Act with regards to standard (universal) precautions, aseptic technique, safe handling and disposal of sharps, prevention of occupational exposure to blood-borne viruses, isolation of patients and disinfection. Infection prevention and control must be included as appropriate in training development plans, learner outcome plans and be robustly recorded through an effective and accessible training records system All staff have a responsibility to ensure they are up to date and competent in all aspects of infection prevention and control within their scope of practice (e.g. Decontamination procedures, aseptic technique and hand hygiene)
Individual Accountability and Responsibility #
Ops Manager
Has a key role in ensuring that systems are in place and being adhered to, to manage any significant risks facing the organisation and ensure compliance with government guidance and legislation. The Ops Manager is ultimately responsible for infection control measures, a responsibility which is discharged through the clinical director
The Ops Manager will be aware of legal duties to identify, assess and control risks of infection in the workplace.
The Training Manager #
The Training Manager will:
- Oversee control of infection policies and their implementation
- Be responsible for the infection control service provision within K4 Medical Services
- Have the authority to challenge inappropriate clinical hygiene practice
- Assess the impact of all existing and new policies and plans on infection and make recommendations for change
- Act decontamination lead has responsibility for the maintenance of a clean safe healthcare environment including the decontamination of medical devices.
- Lead on the development, review and communication of infection prevention and control issues
- Providing support and guidance to assist with compliance
- Identifying and alerting the Ops Manager to changing priorities if and when necessary
- Responsible for ensuring that all staff (clinical and non-clinical), receive education, information and training in infection prevention and control appropriate to their job role.
- Responsible for ensuring that all staff have a working knowledge of infection prevention and control guidance and procedures detailed within this policy.
Logistics Manager
The logistics Manager will/is:
- Responsible for managing the cleaning and decontamination of vehicles and medical equipment during the vehicle deep cleaning process.
- Responsible for the management of laundry services / facilities and of uniform supplies.
- Responsible for ensuring the effective implementation and monitoring of infection prevention and control.
- Responsible for ensuring that ambulance vehicles and equipment are cleaned appropriately and achieve a high standard of cleanliness through a visible presence and are designated as the responsible manager for the routine decontamination of equipment within their area (with the exception of the deep clean process)
- Responsible for ensuring that Staff have access to and are aware of the policies and procedures relating to infection control.
- Report any issues in relation to infection control to the training manager or directly to the company director.
- Establish a cleanliness culture across their areas of responsibility and ensure high levels of cleanliness throughout the organisation.
- Responsible for providing supervision and support. Communicate a vision of cleanliness, challenge poor practice and recognise achievement.
- Act as a role model for infection control practices
All Individuals Employed #
All Individuals Employed / Contracted
Have a personal responsibility to:
- Comply with hand hygiene standards in line with the clean your hands campaign
- Participate in infection prevention and control practices
- Remind colleagues of their infection control responsibilities if there is a potential or actual breach of policy
- Comply with K4 Medical Services Cleanliness and Infection Control policy
- Comply with the wearing of protective infection control equipment (PPE) where exposure to body fluid is a risk.
Standard Infection Control Precautions #
Standard infection control precautions are the constant procedures in place for every patient, clinical staff member and the environment in which healthcare takes place. Application of standard precautions will assist in breaking the chain of infection so reducing the risk of transmission from one patient to another or from patient to staff member and visa-versa. The blood, body fluids, secretions and excretions of patients in any Health care setting may contain either a blood borne virus or other pathogens. It is not always possible to determine the risk posed by individual patients until the results of microbiological and viral investigation is known. Therefore it is recommended that all patients are considered to be a risk for cross infection and that a system of universal or standard precautions must be adopted by all healthcare workers who have direct patient contact and exposure to blood or body fluids. The main role of standard precautions is to protect the healthcare worker from infection and reduce opportunities for transmission of micro-organisms from patient to patient.
There are eight key elements to universal/standard precautions all of which when appropriately implemented are designed to reduce risk of transmission of microorganisms
- Hand hygiene
- Personal protective equipment
- Sharps disposal
- Waste disposal
- Linen handling and segregation
- Blood and body fluid spillage procedure
- Handling and transport of specimens
- Decontamination of equipment and the environment
List of Potentially Infected Substances #
The following table provides guidance on body fluids which may pose a risk of transmission of microorganisms and must be handled with the same precautions as blood:
- Cerebrospinal fluid
- Peritoneal fluid
- Pleural fluid
- Pericardial fluid
- Synovial fluid
- Amniotic fluid
- Semen
- Vaginal secretions
- Breast milk
- Vomit
- Urine
- Any other body fluid, including saliva when in association with dentistry
- Unfixed tissues and organs
An infectious disease can be transmitted by:
DIRECT CONTACT e.g. physical contact with an infected site, such as contact with discharge from wounds or skin lesions e.g. shingles, impetigo
INDIRECT through sneezing or coughing, or when an intermediate carrier is involved in the spread of pathogenic microbes from the source of infection to another person.
Examples include:
Hands – for any healthcare worker are the most important vehicles of cross- infection.
Fomites – are defined as any object which becomes contaminated with organisms from a patient or member of staff which can potentially then transmit them to another person e.g. bedpans, urinals, thermometers, oxygen masks, or practically any inanimate object. The object could be used directly on another patient or could contaminate the hands of healthcare workers.
Aerosols –produced by sneezing or from the dispersal of skin scales can spread through the air and infect others e.g. chicken pox, mumps and measles. The common cold and influenza are often cited as examples, but it is likely that hands and fomites are also important in the spread of respiratory viruses.
Ingestion – infection can occur when organisms capable of infecting the gastrointestinal tract are ingested. When these organisms are excreted faecally by an infected person, faecal-oral spread is said to occur. Organisms may be carried on fomites, hands or in food and drink e.g. Hepatitis A, salmonella, Campylobacter.
Inoculation – infection can occur following a ‘sharps’ injury when blood contaminated with, for example Hepatitis B virus, is directly inoculated into the blood stream of the victim, thereby causing an infection. Inoculation includes blood splashes to the eye. Bites from humans can cause infection by the inoculation mode, and rabies can be spread from infected animal bites. Insertion of invasive devices such as venous and urinary catheters into sterile areas also provides an enormous opportunity for infection. Many intensive care units for example, will immediately replace venous lines that have been inserted in sub-optimal conditions e.g. in an emergency, and reinsert them in aseptic conditions to lower the risk of infection.
Vectors – are any intermediate agent which can carry an infection between humans/other animals. Examples include mosquitoes and leptospirosis.
Absorption – this is not a route of entry for infection except in some tropical diseases.
Risk Assessment Guide for Selection of Protective Equipment Based on Risk of Exposure to Blood / Body Fluid #
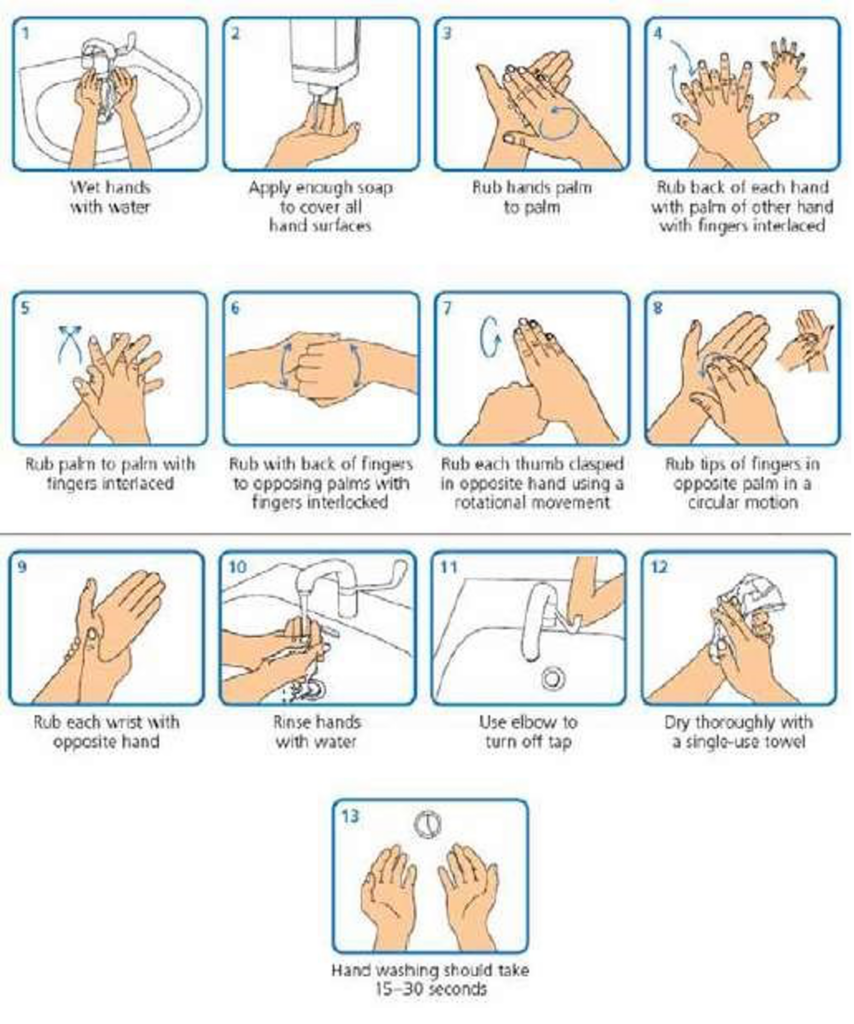
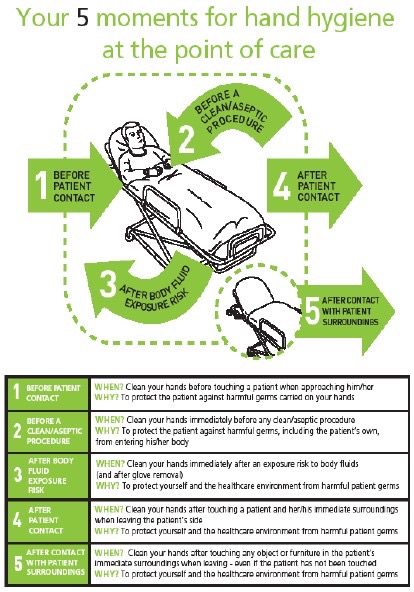
Hand Hygiene Standards for Clinical Staff
Hand hygiene is widely recognised as the single most important activity for minimising the risk of healthcare associated infection. The following four standards are the minimum requirements for both effective hand hygiene and to reduce contamination of frequently handled equipment such as patient monitoring and medical records.
Long Sleeved Jackets should be removed or sleeves shortened to mid forearm for and washing – This is easier to achieve when the weather is warm, but do be aware that particularly fleece sleeves will easily become contaminated, impede access to the wrists and prevent a thorough hand wash
Use the hand gel at the entrance of hospital departments and ask those with you to do the same – This will reduce the contaminates on your hands and set the example for colleagues and relatives accompanying your patient Clinical staff could wear / carry portable gel for use during domiciliary care.
Only freshly donned gloves may be worn within hospital departments or during aseptic procedures – Gloves must not be worn whilst bringing a patient into a hospital department. The only permitted exceptions are when in contact with body fluids and time critical admissions Gloves must not be worn continually but changed between ‘clean’ and ‘dirty’ procedures.
Wash your hands before you leave a hospital department or when you have access to a hand wash basin – Hand washing will remove any soiling making subsequent use of the hand gel more effective.
Personal Protective Equipment (PPE) #
For the purposes of this policy, Personal Protective Equipment (PPE) is defined as being all equipment that is intended to be worn or held by a person at work, which protects them against the transmission of microorganisms and blood-borne viruses. Employees have a responsibility to wear PPE that has been provided by the K4 Medical Services or themselves and to co-operate with management on matters of health and safety. The Protective Personal Equipment at Work Regulations (1992) requires that personal protective equipment is to be supplied and used at work wherever there are risks to health and safety that cannot be adequately controlled in other ways. The regulations also require that PPE:
- is properly assessed before use to ensure it is suitable
- is maintained and stored properly
- is provided with instructions on how to use it safely and
- is used correctly by employees
Selection of protective equipment must be based on an assessment of the risk of transmission of microorganisms to the patient or to the carer, and the risk of contamination of the healthcare practitioners’ clothing and skin by patients’ blood, body fluids, secretions or excretions. Many clinical activities involve no direct contact with body fluid and do not require the use of protective clothing, for example, taking a pulse, blood pressure or temperature.
Staff must use their judgement in determining the likely requirements in each case.
What to Wear and When #
No exposure to blood/body fluids anticipated – no protective clothing required
Exposure to blood/body fluids anticipated, but low risk of splashing – wear gloves and plastic apron
Exposure to blood/body fluids anticipated, high risk of splashing – wear gloves, plastic apron and eye/mouth/nose protection
Types of PPE #
Rubber Gloves
Rubber general purpose gloves should be worn for any domestic cleaning procedure or heavy duty vehicle cleaning. After use they should be washed with detergent and water and dried. When dealing with blood/body fluids, or after infected cases, these gloves should be disposed of in the clinical waste.
Disposable Gloves
Sterile non-latex gloves must be worn for aseptic procedures and contact with sterile sites. Non-sterile, nonlatex examination gloves must be worn for contact with non-intact skin, mucous membranes, all activities that have been assessed as carrying a risk of exposure to blood, body fluids, secretions and excretions and when handling sharp or contaminated instruments. Gloves must be worn as single use items. They are put on immediately before an episode of patient contact or treatment and removed as soon as the activity is completed. Gloves are changed between caring for different patients, or between different care/treatment activities for the same patient. Gloves must be disposed of as clinical waste. Hand hygiene (gel) should precede the donning of gloves and hands decontaminated, ideally by washing with liquid soap and water after the gloves have been removed.
Disposable Apron / Tyvek Suits
Plastic aprons / Tyvek® Suits must be worn when close contact with the patient, materials or equipment are anticipated and when there is a risk that clothing may become contaminated with pathogenic microorganisms or blood, body fluids, secretions or excretions, with the exception of perspiration, or when cleaning the ambulance and equipment. Plastic aprons / Tyvek® Suits must be worn as single-use items, for one procedure or episode of patient care, and then discarded and disposed of as clinical waste. Coveralls are not required routinely except where there is a risk of extensive splashing of blood, body fluids, secretions or excretions, with the exception of perspiration, onto the skin or clothing of healthcare personnel (for example when assisting with childbirth) or when dealing with infections caused by more hazardous organisms or chemical spills. Staff must always ensure they have at least one complete spare uniform available for occasions when uniform contamination has occurred.
Visors / Eye Protection
These are required to be worn when a particular procedure is likely to cause splashing of body fluids, particularly blood or tissue, into the eyes or face. Eye protection is also recommended when caring for patients suspected to be suffering from Severe Acute Respiratory Syndrome (SARS). Following use, eye protection should be disposed of as clinical waste.
Face Masks
Masks offer protection against splashing of the mouth and face. Use of face masks and goggles / visor is recommended during procedures when there is likely to be splash of blood or tissue into the mouth, or if the patient is prone to episodes of coughing or sneezing, or during intubation of patients who are suspected to have meningococcal disease, and in cases of suspected pulmonary tuberculosis (TB). Where patients have an uncontrolled productive cough (cannot cough into a tissue), consideration should be given to encouraging the patient to also wear a face mask. High efficiency masks or respirators with filtering efficiency of the European Standard CEN P2 FFP3 are recommended when caring for patients suspected to be suffering from Severe Acute Respiratory Syndrome (SARS) or Swine Flu. Use of high efficiency masks requires specific training and fit testing under COSHH regulations. They cannot be used by individuals who have a beard or large moustache (or anything that interferes with the fit).
Procedure for Patient Transport Services #
- Before accepting any patient for transportation, the initiating establishment must be asked if the patient has any medical conditions that may cause a significant risk of cross infection to another person
- Patients that pose a significant infection control risk must be transported individually and the accompanying staff should employ PPE if appropriate
- Providing the vehicle is decontaminated daily or immediately following visible contamination the risk of cross infection will be minimised
- Patients suffering from diarrhoea and / or vomiting should avoid non urgent travel until their symptoms have settled. Infected wounds ideally should have clean dry dressings applied. Further advice if required, should be sought from the patient’s healthcare team
- Any concerns regarding infection control issues must be addressed with the initiating establishment, healthcare staff or their infection control team.
Effective communication between health care professionals will enable suitable measures are in place in order to minimise infection risks to both staff and other patients.
Vehicle Cleaning #
It is important to maintain high standards of hygiene within the ambulance to prevent the spread of infection.
All staff have an individual responsibility to keep the ambulance clean and thus to reduce the risk of cross infection to themselves, their colleagues and their patients.
This can best be achieved by all crew members participating in frequent and routine cleaning activities –most importantly between each patient.
A suitable cleaning plan for each vehicle should be designed, agreed and maintained by staff and monitored by managers on a regular basis. No call should ever be delayed as a result of a vehicle being washed or cleaned. Crews must use their judgement in determining the most appropriate time to attend to vehicle and equipment cleaning in order to avoid any disruption to the vehicles deployment.
The Vehicle Exterior
The exterior surfaces of all ambulance service vehicles should be maintained in a consistently clean and hygienic condition. Vehicle wash facilities on stations should be utilised as necessary. The use of PPE should also be considered whenever it is deemed necessary. If pressures of operational requirements prevent a thorough cleaning of the vehicle exterior, attention should be prioritised to the relevant safety and legal requirements ie windscreen, windows, lights, indicators, reflectors, mirrors and number plates. In addition cleaning should pay particular attention to any areas where dirt is likely to be transferred to the crew’s’ hands e.g. door handles. The usual detergent based cleaning agents are satisfactory for general exterior vehicle cleaning; however, if the exterior has become contaminated with blood or body fluids, the detergent clean should be followed by disinfection to eradicate the potential source of infection. PPE (disposable gloves and apron) should be worn in this case and these items must be disposed of into the yellow clinical waste bag.
Vehicle Interior Cleaning – After Each Patient Journey
Vehicle and equipment cleaning should take place after each patient episode. It is good practice to use detergent wipes in order to clean all surfaces that may have been contaminated, including stretcher handles and clinical surfaces. This need only take a few minutes. Blankets, pillow cases, sheets etc must be changed between patients if used. Where an ambulance has become contaminated with blood or body fluid, cleaning must take place following dispatch of the patient at their destination and prior to the next call of duty. Decontamination should normally be carried out where there is access to hot water and cleaning equipment. However, where the spillage is small this can be dealt with using the decontamination equipment carried by all vehicles. Disposable cloths and paper towels should be used for management of blood and body fluid spillages.
The Vehicle Interior – Daily Clean
Using a designated mop, the floor should be cleaned with a fresh hot water and detergent solution. If the mop becomes contaminated with body fluids, it should be changed immediately. Clinical waste bags should be placed in a clinical waste bin, at the receiving hospital. Where this is not possible they should be disposed of at the earliest opportunity. At the end of a shift clinical waste bags are not to be left on a vehicle, they must be removed, tied and put in the appropriate place for collection. Sharps boxes may be left on the vehicle but should be in the closed position. The interior of the vehicle should be checked for sharps and other discarded clinical waste and removed.
Vehicle Interior Cleaning – Monthly Basis
All ambulance interiors should be subjected to a comprehensive clean on a monthly basis. It is accepted that operational demands are likely to restrict opportunities for a weekly clean to be undertaken at a designated time. The arrangements should form part of the cleaning rota designed and agreed with staff to ensure that each vehicle is cleaned on a regular basis. Detachable items should be removed in order that all surfaces can be accessed for cleaning. Ensure that appropriate items of PPE are worn and the vehicle is well ventilated. All walls, ceiling and the inside of cupboards can then be cleaned. Usually a general detergent clean using disposable towels or cloths will suffice, however any areas visibly contaminated with blood or body fluids should be cleaned with the appropriate disinfecting agent. The use of the Narcospray disinfection system then also to be used, following the user manual with the machine.
Cleaning Materials and Equipment Colour Coding #
The colour code below is for cleaning materials. All cleaning items, for example, cloths (re-usable and disposable), mops (these should be changed frequently to avoid using a dirty one. The company have a mop exchange process whereby mop heads are replaced monthly and recorded on a schedule), buckets, aprons and gloves, should be colour coded. This also includes those items used to clean catering departments.